This guide explains when corneal ring segments may help, what tests determine suitability, what results are realistic, and when urgent review is needed.
Last updated: 06/01/2026
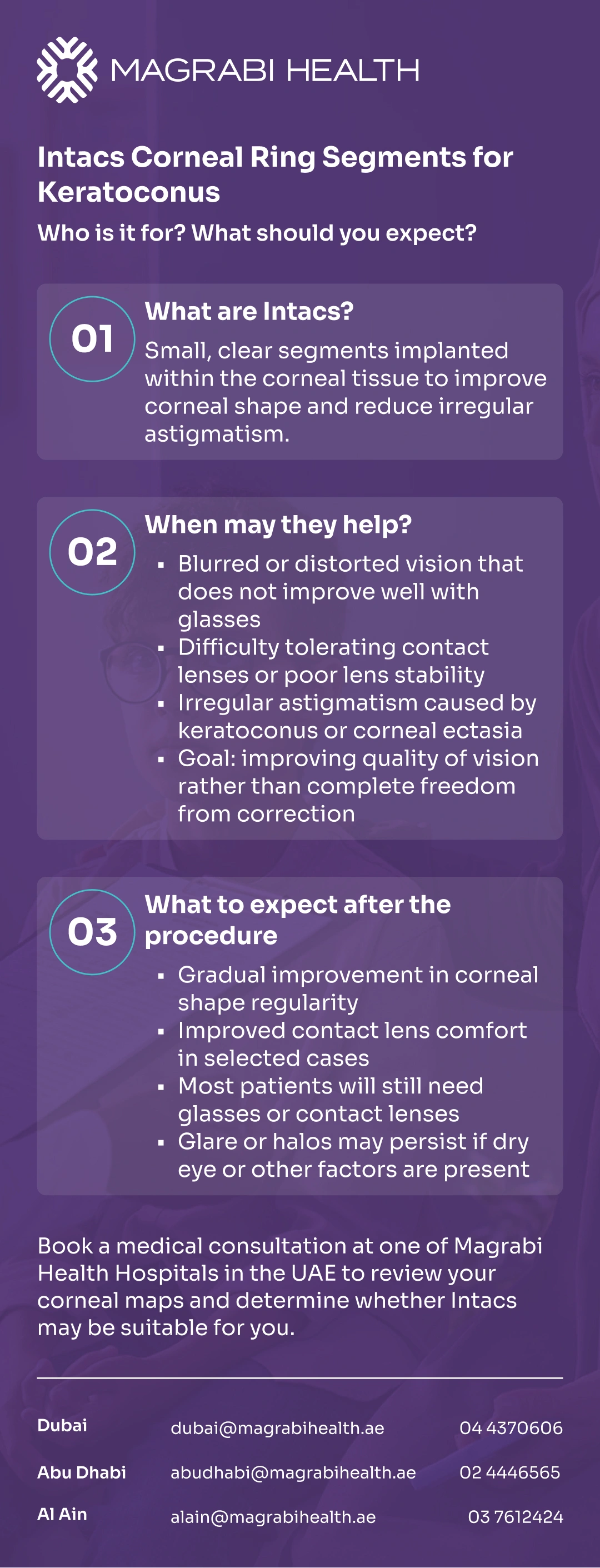
Intacs (intrastromal corneal ring segments, ICRS) are small, clear implants placed within the cornea to reshape it and reduce irregular astigmatism—most commonly in keratoconus or corneal ectasia.
If glasses no longer give you stable clarity, or contact lenses are becoming uncomfortable—especially with long screen hours and night driving glare—your specialist may discuss Intacs as a “shape-improving” option rather than a one-step cure.
This guide explains when corneal ring segments may help, what tests determine suitability, what results are realistic, and when urgent review is needed.
Ready for a decision based on your corneal maps? Book a medical consultation at one of Magrabi Health Hospitals in the UAE to review your scans and discuss whether Intacs may fit your treatment plan.
Intacs are two small arc-shaped segments—often described as an intrastromal corneal ring—placed into the corneal stroma (the middle layer), outside the central optical zone.
By “adding” structure in the corneal periphery, they can flatten and regularize the corneal surface to reduce irregular astigmatism and improve functional vision.
A key point: Intacs are usually intended to improve quality of vision and sometimes contact lens tolerance—not to guarantee perfect vision without glasses.
Intacs—also searched as intracorneal ring segments for keratoconus—are most often considered when the main problem is an irregular corneal shape (such as keratoconus or ectasia) that glasses can’t fully correct.
Common scenarios where Intacs may be discussed include:
You have keratoconus/ectasia with irregular astigmatism affecting daily function (a common reason people search for corneal ring keratoconus options).
You can’t achieve adequate functional vision with glasses or contact lenses anymore, or lenses have become difficult to tolerate.
The goal is to improve corneal shape and day-to-day clarity, not necessarily eliminate all need for correction.
You want to explore a less invasive step that may help defer a corneal transplant in selected cases.
Not every cornea is suitable for ring segments. Your specialist uses scans and clinical findings to judge safety and potential benefit.
Selection is individualized, and questions about corneal rings types often come down to corneal map patterns, thickness, and the surgeon’s planning goals.
A doctor may consider Intacs if you meet several criteria used in clinical practice and labeling, including being an adult and having enough corneal thickness at the planned incision site.
They also typically look for:
A clear central cornea (because central scarring may limit visual improvement).
A corneal shape pattern where reshaping is likely to help (based on tomography/topography).
Symptoms that match the problem: distorted vision, ghosting, glare, or unstable refraction.
Your specialist may avoid or delay Intacs if the cornea is too thin at the intended area, if there are ocular conditions that raise risk, or if other factors make outcomes less predictable.
Also, some patients with large pupils in low light can be more prone to night-vision symptoms after surgery and should be counseled carefully.
Bring what helps your doctor match the plan to your real life:
Your latest glasses prescription(s) and contact lens details.
A brief note on when symptoms worsen (night driving, air-conditioned office, long screen sessions).
Any history of eye rubbing, allergies, or prior eye procedures.
The decision is scan-driven and safety-first. Your evaluation commonly includes several elements.
Doctors typically rely on:
Corneal topography/tomography to map shape, cone location, and irregularity (and to plan segment selection/position).
Corneal thickness measurements and safety margins at the proposed incision/track.
Refraction and vision testing to understand how much is “shape-driven” vs. other causes.
Slit-lamp exam to assess corneal clarity and ocular surface.
Dry eye / tear film assessment, because an unstable tear film can amplify glare and fluctuating blur—common with screens and A/C.
Progression assessment; if progression is suspected, your specialist may prioritize corneal cross-linking (CXL) to stabilize the cornea.
Intacs implantation is usually planned around your corneal maps. The segments are inserted into channels created within the corneal stroma, and the device is designed so it can be removed or replaced if needed.
After surgery, it’s common for vision to fluctuate while the cornea settles. Follow-up visits matter because they confirm healing, ring position, and whether the ocular surface needs extra support (lubricants, allergy control, dry eye treatment).
Results vary because keratoconus/ectasia varies. A realistic goal is “better functional vision” and sometimes easier fitting of specialty contact lenses—rather than a guarantee of spectacle independence.
You can also visit the Refractive and Cornea Care service page on the Magrabi Health website to understand what a corneal mapping and refractive assessment typically includes for keratoconus and irregular corneas.
Many patients notice improvement in:
Corneal shape regularity (less irregular astigmatism).
Quality of vision (less distortion/ghosting in some cases).
Contact lens tolerance or fit in selected patients (because the cornea becomes more regular).
It’s important to plan for what Intacs may not do:
You may still need glasses or contact lenses afterward.
Night glare/halos may persist, especially if tear film instability, large pupils, or other factors contribute.
If progression continues, stabilization (often with CXL) may still be needed.
Vision can stabilize gradually. Your doctor will advise when it makes sense to recheck refraction or refit lenses—based on healing, scan stability, and symptoms.
For an overview of Intacs candidacy and corneal mapping, visit the Refractive and Cornea Care service page on the Magrabi Health website.
Think of Intacs as one tool in a staged plan:
CXL aims to stop keratoconus/ectasia from getting worse, but it does not “return the cornea to normal.”
Specialty lenses (RGP/scleral) may still be the best way to maximize visual acuity, even after ring segments.
In advanced disease or scarring, corneal transplant options may be discussed.
Your plan should match both the scans and your lifestyle demands (night driving, screen exposure, dry environments).
Most surgeries have trade-offs. Intracorneal ring segments complications can include infection/inflammation, ring migration, and (less commonly) extrusion over time.
Seek urgent eye review if you notice:
Worsening pain, or a sudden drop in vision.
Increasing redness, discharge, or marked light sensitivity.
New or rapidly worsening foreign-body sensation.
Signs of ring exposure/protrusion or a persistent epithelial defect (your doctor checks this at the slit lamp).
If Intacs are not the right fit, you still may have options depending on the scans and goals.
Common alternatives include:
Optimizing dry eye treatment and refraction first (often improves glare more than expected).
Specialty contact lenses (especially scleral lenses).
Corneal cross-linking (CXL) if progression is suspected.
Corneal transplant options in advanced scarring/thinning when other methods can’t restore functional vision.
Intacs corneal ring segments can be a practical option when irregular corneal shape is the main reason your vision is distorted—and when the goal is improved functional vision, not a “perfect vision” promise. The best outcomes come from careful scan-based selection, realistic expectations, and a plan that also addresses stability (CXL when needed) and ocular surface health.
If your glasses no longer feel “reliable,” book a cornea and refractive assessment at Magrabi Health Hospitals to review your corneal maps and discuss whether Intacs belongs in your keratoconus plan.
This article is for general education and does not replace an in-person eye examination. Treatment decisions depend on corneal scans, eye health, and individual risk factors. If you have sudden vision loss, severe pain, or increasing redness, seek urgent medical care.
U.S. FDA — Summary of Safety and Probable Benefit for INTACS® Prescription Inserts for Keratoconus (H040002).
American Academy of Ophthalmology (AAO) — Corneal Cross-Linking (patient education).
Moorfields Eye Hospital (NHS) — Corneal cross-linking information (PDF).
NICE — Photochemical corneal collagen cross-linkage for keratoconus (IPG466).
EyeWiki — ICRS extrusion management (complications and warning signs).
American Optometric Association (AOA) — Keratoconus overview. American Osteopathic Association
Reviewed by Dr. Moataz Sallam, Consultant Cataract, Refractive and Anterior Segment Surgeries, with 20+ years of experience in phaco-refractive and cornea care in Dubai and Al Ain.

Step-by-Step Guide to Refractive Surgery Evaluation at Magrabi

What Are Refractive Errors? Causes, Types and Symptoms Explained