If you’ve been told your cornea is “too thin” for LASIK, you may still have safe alternatives. Learn how specialists assess corneal scans and explore PRK, SMILE, ICL, and staged options for thin corneas and keratoconus at Magrabi Hospital.
Last updated: 22/12/2025
If you’ve been told your cornea is “too thin” for LASIK, you still may have safe alternatives. This guide explains how specialists in the UAE evaluate corneal scans, dry eye, and lifestyle factors before recommending vision correction for thin corneas.
Hearing “you’re not a LASIK candidate” can be frustrating—especially with night driving and long screen hours in air-conditioned settings.
A careful assessment can clarify why LASIK isn’t advised and which options, such as PRK, SMILE, or ICL, could fit you.
Ready to explore your options? Book a refractive consultation with a Magrabi Health eye specialist to review your scans and discuss a plan tailored to your needs.
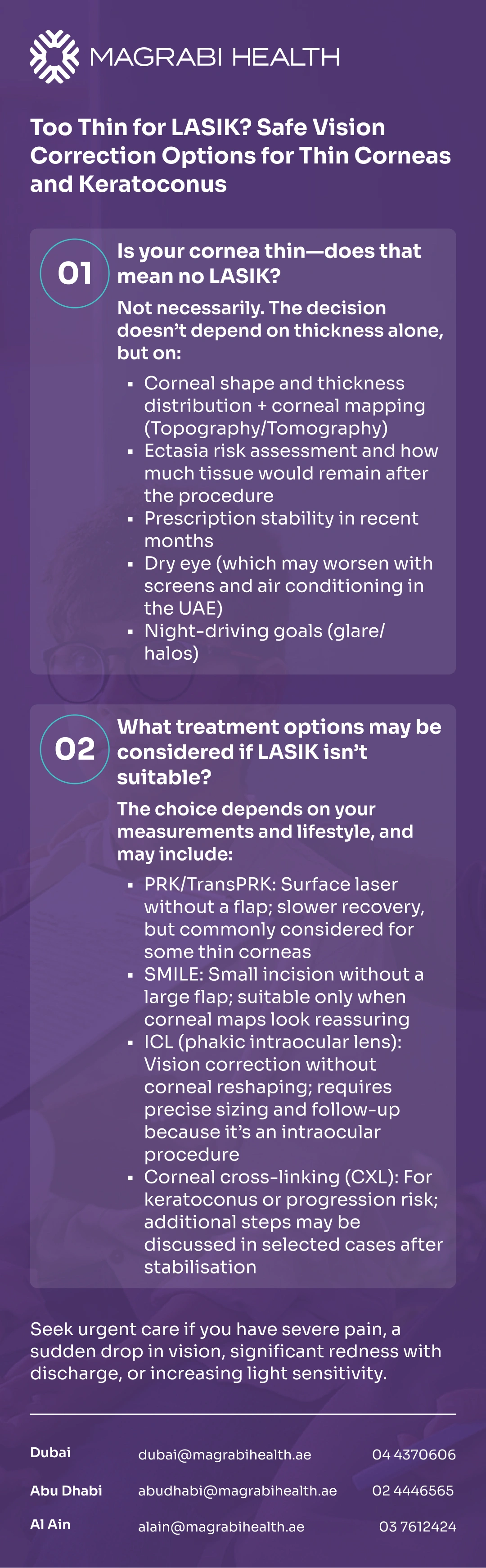
“Thin cornea” is not a diagnosis—it’s one piece of a larger safety puzzle. The key question is whether reshaping the cornea would leave it stable enough long term, especially in eyes with early keratoconus (a condition where the cornea becomes thinner and changes shape over time).
In practice, “too thin” often means one of these: you may need a large correction, your cornea’s shape raises concern for weakness, or the predicted remaining corneal tissue after a flap-and-laser procedure could be inadequate.
That’s why reputable clinics focus on risk profiling—not just a single thickness number—before recommending vision correction for thin corneas.
A proper eligibility decision is based on a set of measurements that work together. This is where advanced corneal imaging and a thorough eye-surface evaluation matter most when thin corneas are part of the picture.
Thickness is measured (often with pachymetry) and combined with how much laser reshaping is planned.
Surgeons also consider how much supportive corneal tissue would remain after creating a flap, because a thinner remaining structure can raise the risk of corneal weakening (ectasia) in susceptible eyes.
The important takeaway is simple: two people can have the same thickness, yet different safety profiles depending on corneal shape, prescription, and other risk factors.
Topography and tomography map the cornea’s curvature and thickness pattern.
This helps detect irregularities and early keratoconus patterns that might not be obvious on a standard eye test. Abnormal pre-operative maps are a well-known risk signal for post-laser ectasia, which is why detailed screening is a cornerstone of safer refractive care.
If your maps look suspicious, your surgeon may recommend avoiding flap-based LASIK and discussing alternative vision correction for thin corneas.
Even with “good scans,” LASIK may be delayed or avoided if your prescription is changing, or if dry eye is significant—because dryness can affect comfort and the quality of vision, particularly with heavy screen use and UAE air conditioning.
Guidance from health authorities also emphasizes that not everyone is an ideal candidate and that alternatives exist.
Night driving goals matter too: some people are more sensitive to glare and halos during healing, so your surgeon should factor this into the choice and counseling.
There are common scenarios where LASIK is often not the safest first choice. Your surgeon should explain which factors apply to you and why.
Suspected or confirmed keratoconus, or an irregular corneal shape on imaging
High ectasia risk signals on topography/tomography (even if vision seems “okay” today)
Thin cornea relative to the amount of correction planned, meaning less supportive tissue would remain
Significant, untreated dry eye or ocular surface disease
Unstable prescription or certain eye/health conditions where safety is not established
If you recognize yourself in any of these, it doesn’t mean “no options.” It means the plan should shift toward safer alternatives.
If LASIK is not advised, the goal becomes choosing a method that meets your vision needs while respecting corneal strength and surface health. Below are common alternatives discussed in modern vision correction for thin corneas.
PRK reshapes the cornea without creating a flap. Instead, the surgeon works on the surface layer, which then heals over time.
The AAO explains PRK as a laser option that corrects refractive error by reshaping the cornea after surface preparation and careful measurements.
What patients often notice is that recovery feels slower than LASIK: discomfort, light sensitivity, and blurry vision can be more noticeable in the first days, and vision may fluctuate during healing.
That said, PRK is frequently considered when a flap is less desirable, and it’s a well-established part of vision correction for thin corneas when appropriate.
SMILE is a small-incision laser procedure that avoids a large flap. For some people, it may reduce certain flap-related concerns.
However, it is not automatically “better” for every thin-cornea case—because safety still depends on corneal shape, thickness distribution, and ectasia risk screening.
If your scans show keratoconus patterns, the priority is often stabilisation rather than laser reshaping. In that situation, SMILE may still be avoided, and other vision correction for thin corneas may be safer.
A phakic intraocular lens (often called ICL) is placed inside the eye without removing your natural lens. Because it does not reshape the cornea, it can be an attractive option for vision correction for thin corneas in selected patients—especially when corneal laser options are limited.
Like any intraocular procedure, it has risks and requires careful sizing and follow-up. The FDA provides patient information about benefits and risks of phakic intraocular lenses, and notes that there may be risks not yet fully known with newer technologies.
Refractive lens exchange replaces the eye’s natural lens with an artificial lens, similar to cataract surgery. It may be considered in selected patients, typically when lens-based factors (such as early cataract changes or age-related needs) make it a more logical solution than corneal laser.
The NHS discusses laser eye surgery alongside lens surgery options and potential complications.
Because this is intraocular surgery, it is not the first choice for many younger patients, but it can be part of the broader conversation around vision correction for thin corneas.
You can also visit the Refractive and Cornea Care service page on the Magrabi Health website to learn what a refractive assessment includes and which procedures may be offered.
If keratoconus is present, the conversation shifts from “best laser procedure” to “stabilise first, then improve function.” Keratoconus involves progressive thinning and a cone-like change in corneal shape that can blur and distort vision.
In many cases, the safest goal is not perfect unaided vision, but better day-to-day function with glasses, specialty contact lenses, and—when needed—procedures that slow progression.
This framing reduces pressure to pursue high-risk laser reshaping and supports safer vision correction for thin corneas over the long term.
Some patients benefit from a step-by-step approach rather than a single “one-and-done” procedure. This is especially true when keratoconus or ectasia risk is a concern.
Corneal cross-linking (CXL) uses riboflavin drops and ultraviolet light to strengthen corneal collagen bonds. Major clinical guidance describes it as a treatment aimed at preventing keratoconus (or ectasia) from getting worse, rather than restoring the cornea back to normal.
If progression is suspected, CXL may be recommended before considering other vision correction for thin corneas that could stress the cornea.
In some carefully selected cases, surgeons may consider surface laser reshaping after CXL to improve the quality of vision—often with conservative goals and strict safety checks.
This is not for everyone, and timing depends on healing and stability.
The key point is that “laser after CXL” is a personalised medical decision, not a standard package, within vision correction for thin corneas.
If the cornea is stabilised but significant refractive error remains, some patients may be evaluated for ICL after CXL. The logic is to correct vision without further corneal thinning, while still respecting intraocular safety requirements and long-term monitoring.
Outcomes vary by procedure, your prescription, and the health of your tear film. Setting realistic expectations is part of high-quality vision correction for thin corneas.
Speed of recovery: PRK usually takes longer to feel “stable,” while ICL vision may sharpen faster once healing settles.
Night driving: glare/halos can happen during healing; persistent symptoms deserve re-evaluation rather than “waiting it out.”
Dry eye comfort: air conditioning and screen time can worsen symptoms, so treating dryness can improve both comfort and vision quality.
The realistic goal: many procedures aim to reduce dependence on glasses/contacts—not promise “perfect vision.”
Every refractive option has trade-offs. The safest approach is the one that matches your risk profile, not the one that sounds most convenient.
This is especially important when corneal strength is a concern, where ectasia avoidance is a central goal.
Potential issues can include dry eye, glare/halos, slower healing (more common with surface procedures), or intraocular risks with lens implants.
Health agencies also encourage patients to review objective information and discuss eligibility limits with their surgeon.
After any eye procedure—or even during evaluation—some symptoms warrant prompt assessment. Seek urgent care if you have severe or worsening pain, sudden vision drop, marked redness with discharge, increasing light sensitivity, or trauma to the eye.
Being “too thin for LASIK” is often a prompt to get better measurements—not to give up. With modern imaging, careful risk screening, and multiple alternatives, many people can still pursue vision correction for thin corneas in a way that prioritises long-term corneal stability and everyday visual comfort.
If you’re considering the next step, schedule a consultation at Magrabi Hospital to review your corneal scans and discuss a safe, personalised plan.
This article is for general education and does not replace a comprehensive eye examination. Suitability for any procedure depends on individual measurements and medical history; only an eye specialist can advise you after an in-person assessment.
American Academy of Ophthalmology (AAO): Corneal Cross-Linking; What Is Keratoconus?; Photorefractive Keratectomy (PRK).
NHS (UK): Laser eye surgery and lens surgery; patient information on cross-linking.
NICE (UK): Corneal collagen cross-linking guidance for keratoconus/keratectasia.
U.S. FDA: LASIK information pages; risks of phakic intraocular lenses; LASIK Quality of Life (PROWL) information.
ASCRS: Post-LASIK ectasia risk factors and management overview (professional society).
Reviewed by Dr. Moataz Sallam, Consultant Cataract, Refractive and Anterior Segment Surgeries, with 20+ years of experience in phaco-refractive and cornea care in Dubai and Al Ain.