LASIK for keratoconus is often not recommended. This article explains why corneal scars and irregular corneas need different solutions, and how eye specialists decide on safer options.
Last updated: 23/12/2025
LASIK for keratoconus is usually not recommended, because reshaping a weak or irregular cornea can increase the risk of the cornea becoming unstable over time (corneal ectasia). Corneal scars are different: some scars mainly affect “clarity,”
while others change the cornea’s shape and create distorted vision—so the plan depends on where the scar is and how deep it is.
A careful exam and corneal scans are the safest way to decide, especially for people with long screen hours, air-conditioning exposure, and night driving concerns in the UAE.
This guide explains why LASIK is often not the safest choice for these corneas, what tests matter most, and which options eye specialists may discuss instead.
Would you like a clear decision based on your corneal scans? Book a refractive consultation with an eye specialist at Magrabi Health Hospital.
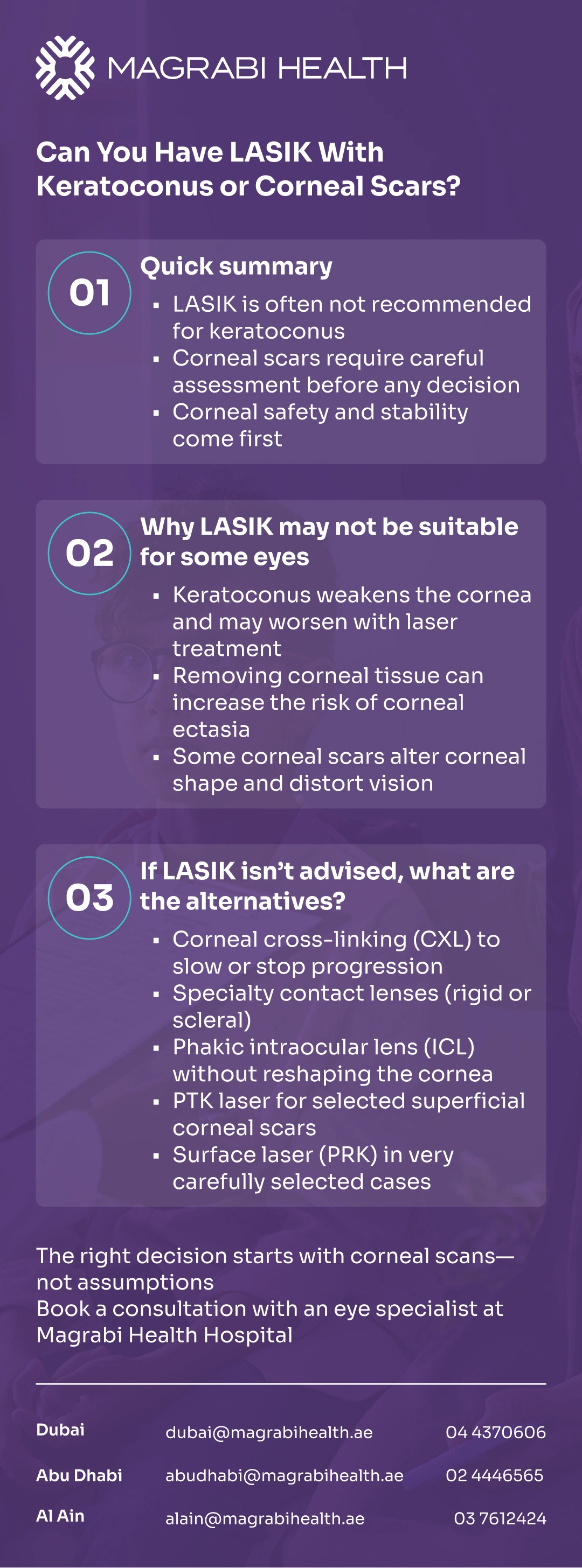
In most cases, keratoconus is a “no” for LASIK because the cornea is already prone to thinning and shape change. Clinical guidance lists keratoconus and other corneal ectasias as contraindications for corneal refractive surgery.
For corneal scars, LASIK may be possible in select situations, but only if the scar does not significantly disrupt the cornea’s shape, healing, or optical quality—something your scans and exam help clarify.
If you have keratoconus (or early/hidden keratoconus on scans), LASIK is generally avoided because it can raise the risk of corneal ectasia (progressive bulging or thinning after surgery).
If you have a corneal scar, the answer depends on the scar’s location, depth, and whether it causes irregular astigmatism—a type of distortion that glasses may not fully correct.
Keratoconus is a condition where the cornea becomes thinner and more cone-shaped over time, leading to irregular astigmatism and reduced visual quality.
LASIK for Keratoconus works by removing corneal tissue to change how the eye focuses. In keratoconus, the cornea may already be biomechanically weak, so removing tissue can increase the risk of long-term instability.
“Stable” usually means your prescription and corneal maps have not meaningfully worsened over time. If progression is suspected, doctors often discuss corneal cross-linking (CXL) first, because it is designed to help stabilise the cornea rather than reshape it.
A corneal scar can result from an injury, infection, inflammation, or previous eye surgery. What matters most is how the scar affects the cornea’s optical quality and surface regularity.
Scars closer to the centre of vision are more likely to reduce sharpness and cause glare or ghosting, especially at night. Some scars mainly scatter light rather than blur vision in a simple way.
Superficial scars may sometimes be managed differently from deeper scars. When a scar is deep or causes significant surface irregularity, laser-based vision correction may not be predictable or safe.
A safe decision is not based on your glasses number alone. It depends on understanding corneal shape, corneal strength, and tear film quality.
These scans show both the front and back surfaces of the cornea and how thickness is distributed. This helps detect keratoconus (including early forms) and explains why two people with the same thickness may not have the same risk.
Specialists assess patterns linked to corneal weakness and confirm whether your vision and scans have been stable over time. This is a key reason LASIK may be ruled out even when vision seems “not too high.”
Dry eye can blur vision and affect comfort after refractive surgery. In the UAE, long screen use and air-conditioning often make symptoms more noticeable, so tear film health is an important part of planning.
If you drive at night, factors such as pupil size, corneal irregularity, and light scatter are reviewed, because irregular corneas can increase glare and halos after laser procedures.
You can also visit the Refractive and Cornea Care service page on the Magrabi Health website to learn what a refractive assessment includes for eyes with keratoconus or corneal scars.
When LASIK is not recommended, the goal is to protect the cornea while improving vision quality as much as possible.
Corneal cross-linking (CXL): Often discussed when keratoconus is progressing, to help stabilise the cornea.
Specialty contact lenses (RGP or scleral lenses): These lenses can neutralise corneal irregularity and often provide clearer vision in keratoconus or scar-related distortion.
Phakic intraocular lens (ICL): An implantable lens option that corrects refractive error without reshaping the cornea.
PTK (phototherapeutic keratectomy): A laser procedure sometimes used for selected superficial corneal scars or surface problems.
Surface laser (PRK or TransPRK): Considered only in very carefully selected cases, with conservative goals and reassuring scans.
If you’d like to explore these options, you can visit the relevant service page on Magrabi Health’s website.
For many people, management happens step by step rather than with one single procedure.
CXL is aimed at reducing the risk of progression. It is not designed to fully correct vision, but it can make future vision planning safer.
After stabilisation, vision may be improved with specialty contact lenses, and in some cases with options like ICL, depending on individual measurements.
In selected cases, intracorneal ring segments may be discussed to improve corneal shape regularity. This is different from LASIK and not suitable for everyone.
With scars, the key question is whether vision problems come mainly from reduced clarity, irregular shape, or both.
If there is any concern about ongoing inflammation or infection, that issue must be treated before considering elective vision correction.
Superficial surface problems may sometimes be managed with PTK, while irregular astigmatism often responds better to rigid or scleral lenses.
In rare and more advanced cases, corneal transplantation may be considered when other options cannot provide useful vision.
It’s helpful to aim for safer and clearer, not instant perfection.
With keratoconus or corneal scars, improving visual quality—such as reducing distortion and glare—can be just as important as lowering your glasses prescription. Some people will still need glasses or contact lenses after treatment.
Seek prompt medical advice if you notice:
A sudden drop in vision or rapidly increasing distortion
New eye pain, redness, or strong light sensitivity
Sudden intolerance to contact lenses or worsening night glare
Eye injury or concern about an eye infection
When considering LASIK for keratoconus or in eyes with corneal scars, the first priority is always protecting the eye and maintaining corneal stability.
LASIK may not be the right choice for every eye, but this does not mean there are no safe alternatives.
With careful testing and detailed corneal scans, an eye specialist can explain which options are most appropriate for your eyes and help improve vision quality step by step—based on medical findings, not assumptions.
Would you like a clear decision based on your corneal scans? Book a refractive consultation with an eye specialist at Magrabi Health Hospital.
This article is for general educational purposes only and does not replace a full eye examination or personalised medical advice. Suitability for LASIK or alternative treatments depends on detailed testing and individual eye health.
American Academy of Ophthalmology (AAO).
Keratoconus and Corneal Ectasia – Patient & Clinical Overview
NHS Moorfields Eye Hospital.
Reviewed by Dr. Moataz Sallam, Consultant Cataract, Refractive and Anterior Segment Surgeries, with 20+ years of experience in phaco-refractive and cornea care in Dubai and Al Ain.