Understanding when symptoms suggest infectious keratitis (corneal infection) or a developing corneal opacity can help you act early and protect vision quality, not just acuity. This guide explains warning signs, what a cornea specialist checks, and realistic corneal scar treatment options.
Last updated: 08/01/2026
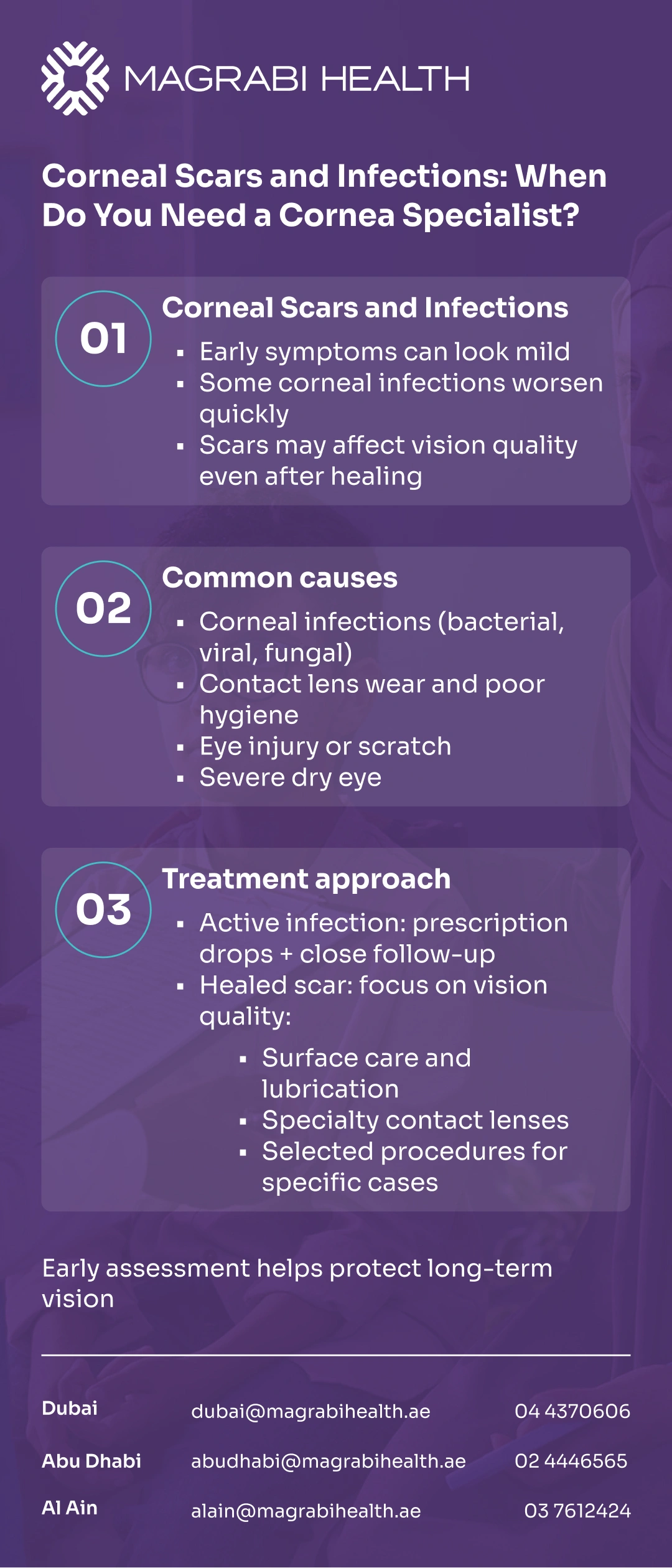
Corneal scars and infections can look “similar” at first—redness, discomfort, blur—but the timeline and risks are not always the same. In some cases, a scarred cornea or early corneal clouding may develop gradually after inflammation.
In the UAE, long screen hours, air-conditioning dryness, and contact lens wear can add to irritation and delay seeking care.
Understanding when symptoms suggest infectious keratitis (corneal infection) or a developing corneal opacity can help you act early and protect vision quality, not just acuity.
This guide explains warning signs, what a cornea specialist checks, and realistic corneal scar treatment options.
Would you like a clear plan based on a microscope examination and corneal imaging? Book a consultation at one of Magrabi Health Hospitals in the UAE to assess your cornea and discuss the next steps.
The cornea is the clear “front window” of the eye. When its surface becomes inflamed, infected, or scarred, light can scatter—causing blur, glare, halos, and reduced contrast (often most noticeable at night), a pattern commonly seen with corneal clouding or corneal opacity.
A corneal infection (often called microbial or infectious keratitis) is when bacteria, viruses, fungi, or (more rarely) parasites infect the cornea, sometimes progressing to a corneal ulcer.
Some infections can worsen rapidly, which is why early assessment matters—especially if pain, light sensitivity, and blurred vision are present. Many patients ask: Are corneal infections dangerous?
Contact lens wear is a major risk factor, particularly with poor hygiene or overnight wear, and is a common cause of corneal infection.
A corneal scar is a “healing mark” left when deeper layers of the cornea are affected—most commonly after an infection, trauma (scratch/foreign body), or significant inflammation. A scar on the cornea from infection is one of the most frequent causes of a corneal ulcer scar.
A scar may be subtle but still cause glare, ghosting, or reduced clarity depending on its depth and location (central vs peripheral).
These symptoms may indicate an active problem related to corneal scars and infections, such as infectious keratitis or a corneal ulcer, and should be assessed urgently—especially in contact lens users.
These are classic signs of corneal infection.
Severe eye pain or rapidly worsening discomfort.
Marked light sensitivity (photophobia).
Red eye with blurrey vision.
A visible white/grey spot on the cornea.
Discharge, watering, or “something in the eye” sensation that is getting worse.
Symptoms not improving as expected after initial treatment.
A cornea specialist is particularly important when corneal scars and infections are suspected—such as when symptoms suggest a corneal ulcer or active infection, when vision is affected, or when a visually significant scar may be developing.
Specialist input is also valuable for contact lens users with pain or redness, or when symptoms related to corneal scars and infections recur or do not improve as expected.
You can also visit the Refractive and Cornea Care service page on the Magrabi Health website to learn what a cornea-focused assessment typically includes.
A cornea visit is usually structured to confirm whether this is dryness/irritation, an abrasion, an active infection, or a healing scar—and how deep it goes.
A slit-lamp microscope lets the doctor examine the cornea in detail, look for an ulcer/infiltrate, measure inflammation, and check for healing patterns.
Imaging can help assess surface regularity and the likely visual impact of scarring, and guide whether conservative treatment or procedures may be considered.
In selected cases—such as larger, central, severe, atypical, or non-responding ulcers—samples (smears/cultures) may be recommended to guide targeted therapy.
Treatment for corneal scars and infections is chosen based on what the cornea is dealing with—an active infection versus a healing scar—and how deep and central the problem is (near the visual axis versus peripheral).
A mild surface irritation or small superficial abrasion is managed differently from infectious keratitis or a deeper ulcer, because the risks and follow-up intensity are not the same.
A mild surface irritation or a small superficial abrasion is often managed differently from infectious keratitis or a deeper ulcer, because the risks—and follow-up intensity—are not the same.
If an infection is suspected, treatment may include prescription antimicrobial drops (sometimes started urgently) and close follow-up to ensure the cornea is improving as expected.
In selected cases—especially if the ulcer is large, central, severe, atypical, or not responding—your specialist may recommend corneal sampling/culture to guide targeted therapy.
When the main issue is a corneal scar after healing, the goal shifts to improving visual quality (blur, glare, ghosting).
Options may range from lubrication and surface care (if dryness contributes) to specialty contact lenses (e.g., rigid or scleral lenses) that can “optically smooth” irregularity.
In very selected cases, certain procedures such as intrastromal corneal ring segments (Intacs) may be discussed, depending on the depth and location of the scar and its impact on visual quality, with realistic visual goals in mind.
Delay can increase the chance that the problem becomes deeper or more central, which raises the risk of persistent scarring, irregular astigmatism, and long-term vision distortion.
Many patients wonder is a corneal ulcer an emergency—and the answer is often yes, when symptoms worsen or vision is affected.
Corneal infections and corneal scars aren’t just “red eye” problems—timing, pain, and vision changes can signal when you need cornea-level evaluation. If symptoms are significant, worsening, or linked to contact lenses, a cornea-focused exam can help protect both sight and visual quality.
If you’re unsure whether this is an infection, an abrasion, or a scar-in-progress, book an eye consultation at Magrabi Health Hospitals in the UAE for a targeted corneal assessment.
This article is for general health education and does not replace an in-person exam. If you have severe pain, sudden vision changes, marked light sensitivity, or a visible white spot on the cornea—seek urgent eye care.
Reviewed by Dr. Moataz Sallam, Consultant Cataract, Refractive and Anterior Segment Surgeries, with 20+ years of experience in phaco-refractive and cornea care in Dubai and Al Ain.
American Academy of Ophthalmology (AAO) — Corneal Ulcer (Keratitis).
American Academy of Ophthalmology (AAO) — Bacterial Keratitis Preferred Practice Pattern (PPP).
NHS (Imperial College Healthcare) — Microbial keratitis patient leaflet.
Moorfields Eye Hospital (NHS) — Microbial keratitis.
CDC — Healthy contact lens wear and infection prevention.
Mayo Clinic — Keratitis: symptoms and causes (Arabic/English versions).