If your vision has become cloudy, distorted, or painful because the cornea is scarred, swollen, or misshapen, your specialist may discuss corneal transplant care (corneal transplant surgery/keratoplasty). This guide explains cornea graft types—full thickness transplant vs lamellar keratoplasty (including DALK and DSAEK)—who may need surgery, and a realistic corneal transplant recovery time timeline.
Last updated: 12/01/2026
If your vision has become cloudy, distorted, or painful because the cornea is scarred, swollen, or misshapen, your specialist may discuss corneal transplant care (corneal transplant surgery/keratoplasty).
In the UAE, long screen hours, air-conditioned dryness, and night driving glare can make symptoms feel more disruptive day to day.
This guide explains cornea graft types—full thickness transplant vs lamellar keratoplasty (including DALK and DSAEK)—who may need surgery, and a realistic corneal transplant recovery time timeline.
Ready to discuss whether corneal transplant in UAE care is appropriate for your eye? Book a consultation with an eye specialist at Magrabi Health Hospitals in the UAE to review your scans and treatment options.
A corneal transplant replaces diseased or damaged corneal tissue with healthy donor tissue to improve vision, reduce symptoms, or both.
Some procedures replace the full thickness of the cornea, while others replace only selected layers (partial thickness / lamellar keratoplasty).
The best approach depends on the layer involved and the cause of corneal damage.
In some cases, the next step depends on scar depth and location, so your doctor may review corneal scar treatment options before recommending keratoplasty.
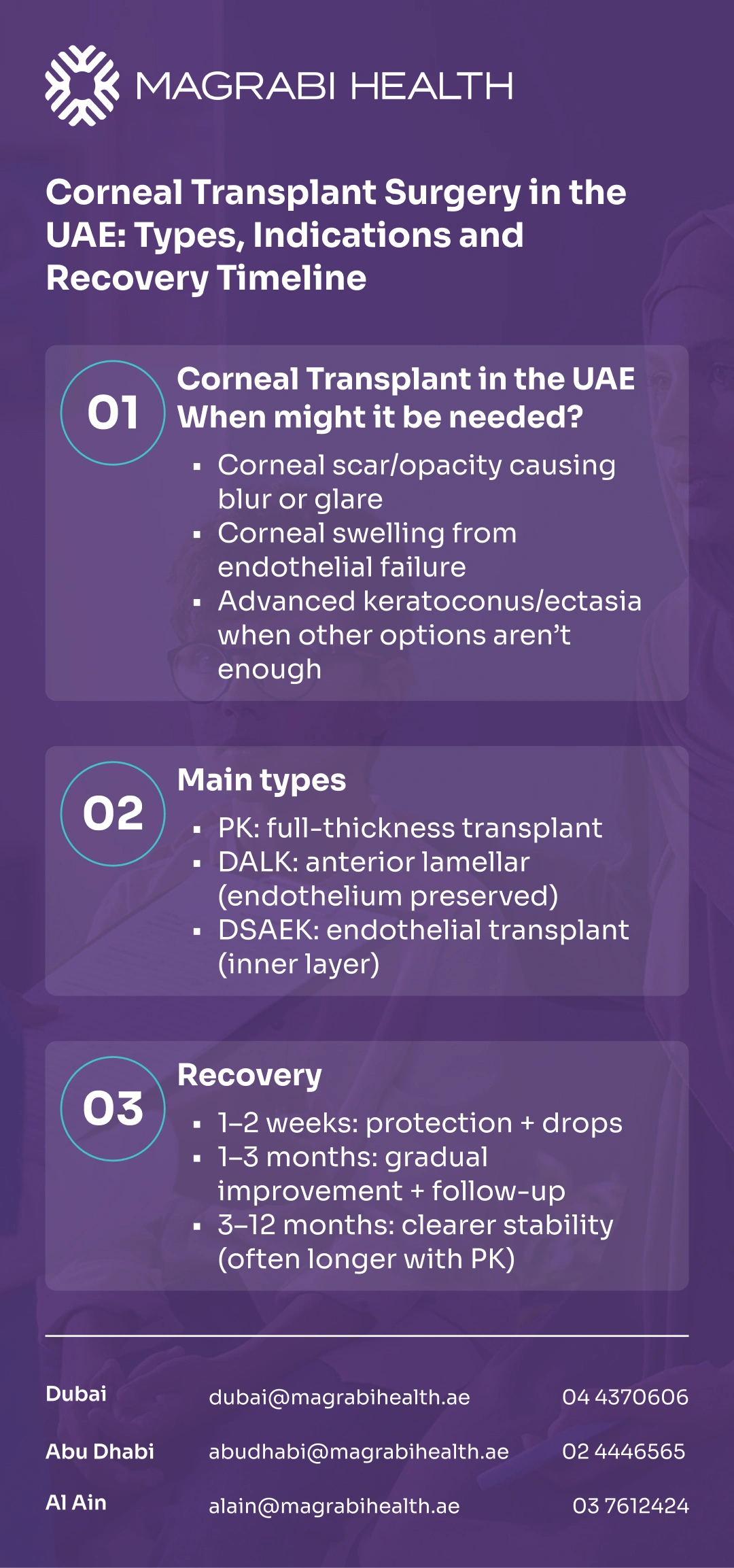
A corneal transplant in UAE is typically considered when the cornea can no longer stay clear or maintain a stable shape with other treatments.
Your doctor will link your symptoms to your corneal findings—not just a vision chart number.
Corneal scarring or opacity that reduces vision quality (blur, glare, ghosting).
Endothelial failure / corneal swelling (the inner pump layer is not working well).
Painful corneal disease where transplant may reduce pain as well as improve sight in selected cases.
Repeat graft (regraft) if a previous cornea graft fails or becomes cloudy again.
Keratoconus or corneal ectasia when vision cannot be stabilised with lenses and other measures.
In selected keratoconus or corneal ectasia cases, Intacs corneal ring segments may be discussed to improve corneal shape and vision quality before moving to transplant.
The goal is to replace only what is needed—and preserve healthy layers when possible. This is why “cornea graft types” matter as much as the diagnosis.
PK replaces all layers of the cornea. It may be considered when scarring or disease affects full thickness tissue, or when partial-thickness options are not suitable.
Recovery can be gradual because sutures and healing influence vision and astigmatism over time.
DALK is a partial thickness corneal transplant in UAE that preserves the endothelium (inner layer) and replaces the front/middle layers.
It is commonly used when the endothelium is healthy—often in keratoconus—so it can be a tissue-sparing option in selected patients.
DSAEK (a form of endothelial keratoplasty) replaces mainly the inner layers (endothelium/Descemet’s membrane with a thin layer of supporting tissue).
It is often used when the primary problem is endothelial failure and swelling rather than surface scarring.
Visual rehabilitation can be faster for many patients compared with full thickness transplant, but suitability depends on the eye’s condition and surgical factors.
Your surgeon typically considers which corneal layer is diseased, how deep any scarring is, whether the eye has had prior surgery, and what your daily needs are (night driving, screen-heavy work, contact lens tolerance).
The “best” corneal transplant in UAE care is the one that matches your corneal maps and risks.
A decision about corneal transplant surgery should come after confirming what is driving blur or discomfort. Many symptoms overlap with dry eye, cataract, or irregular astigmatism, so testing matters.
Specialists commonly use:
Vision/refraction testing and slit-lamp exam.
Corneal topography/tomography (shape and thickness mapping).
Pachymetry, endothelial assessment when relevant.
Ocular surface evaluation (tear film stability, dry eye contributors).
While techniques vary by cornea graft type, the principle is the same: remove the diseased tissue and replace it with donor tissue, then support healing with medications and follow-up.
Your surgeon will explain anesthesia, positioning (especially for endothelial procedures), drop schedules, and activity limits based on your individual plan.
Recovery is rarely “instant.” Vision typically improves in phases, and dryness (air-conditioning + screens) can affect comfort and fluctuations, especially early on.
Early healing focuses on protecting the eye and preventing inflammation/infection. You may have fluctuating blur, light sensitivity, and a “foreign body” sensation depending on the procedure and sutures.
This period is often about stabilising the surface, adjusting medications, and monitoring pressure. Vision may still vary day to day—particularly with dry environments and long screen time.
For full thickness transplant (PK), astigmatism management and suture-related changes can continue for months.
Glasses or contact lenses may be updated as the cornea shape settles. For some partial-thickness procedures, functional vision may stabilise sooner, but follow-up remains essential.
You can also visit the Refractive and Cornea Care service page on the Magrabi Health Hospitals website to understand what a cornea-focused assessment typically includes before planning surgery.
Return-to-activity timing depends on healing, eye pressure, and vision stability.
If night driving is a priority, your doctor will focus on glare control and safety rather than speed. Avoid self-deciding—follow the plan given for your specific corneal graft operation.
Every corneal transplant surgery has risks, and early recognition of problems can protect the graft. Rejection can sometimes be reversed if treated promptly—so knowing the warning signs matters.
Rejection warning symptoms can include redness, light sensitivity, blurred vision, pain/discomfort, and tearing.
Infection/inflammation may present with worsening pain, increasing redness, discharge, or sudden drop in vision.
High eye pressure can occur, sometimes related to steroid drops, and needs monitoring.
If you experience a sudden change—especially worsening redness, pain, light sensitivity, or new foggy vision—contact your surgical team urgently the same day.
Many patients do well after keratoplasty, but outcomes vary by diagnosis, graft type, ocular surface health, and adherence to drops and follow-up. A cornea graft can last many years in suitable cases, but lifelong monitoring may still be needed because rejection or late problems can occur.
Your specialist may also discuss:
Long-term drop plans (often steroid-based for a period)
Managing dryness and eyelid/tear film issues
Vision optimisation (glasses, specialty contact lenses, or further procedures in selected cases)
A corneal transplant in UAE care is not a single moment—it’s a staged plan: confirm the layer involved, choose the right technique (PK vs DALK vs DSAEK), and commit to structured follow-up so the graft has the best chance to stay clear.
If you’re considering corneal transplant surgery, book a consultation at Magrabi Health Hospitals in the UAE to review your corneal maps and discuss cornea graft types, risks, and a realistic recovery timeline.
This article is for general education and does not replace an in-person eye examination or personalised medical advice. If you have severe pain, sudden vision loss, or rapidly worsening redness/light sensitivity, seek urgent medical care.
Reviewed by Dr. Moataz Sallam, Consultant Cataract, Refractive and Anterior Segment Surgeries, with 20+ years of experience in phaco-refractive and cornea care in Dubai and Al Ain.
American Academy of Ophthalmology (AAO) — patient information on corneal transplantation and partial-thickness options (including DALK).
NHS (UK) — cornea transplant overview, recovery and complications.
Moorfields Eye Hospital (NHS) — penetrating keratoplasty patient information and risks (including rejection as a lifelong possibility).
The College of Optometrists — corneal transplant rejection symptoms and urgency of treatment.